By Eric Guroff (Ratio PBC) and Swati Shah Patel (Resolve to Save Lives, an initiative of Vital Strategies)
Context Setting
As the COVID-19 pandemic spread to the United States in Spring 2020, public health departments scrambled to implement proven public health interventions at the massive scale that the crisis demanded. Contact tracing and case investigation (“Test, Trace, Isolate, Support”) is a long-established, effective public health measure used to contain the spread of infectious diseases. However, the people, processes, and technology used to deliver these programs were ill-prepared for the scale of the COVID-19 pandemic seen in the US.
To provide assistance to public health agencies, Resolve to Save Lives (RTSL), a global public health initiative led by former CDC Director Dr. Tom Frieden, and LFPH member company Ratio PBC (Ratio), a public health technology consultancy, collaborated to help scale contact tracing and case investigation methods with technology. Together, RTSL and Ratio partnered with state and county public health departments across the US to design, build, and implement open source digital tools to increase the efficiency of the contact tracing and case investigation workforce and existing case management systems (CMS).
While each infectious disease outbreak is different, our successes and failures through the early stages of the COVID-19 pandemic offer several key lessons for public health leaders and technologists to prepare for future crises.
What We Built
Table 1: Digital Tools Developed in Context of Case Investigation & Contact Tracing Workflow
- Epi Viaduct is a data pipeline that moves test results from state lab reporting systems to case management systems used for case investigation and contact tracing. The system enables teams to more quickly reach, investigate, and contact trace index cases. The lab data transfer and processing time of the states using this tool has successfully decreased from several hours to just seconds. View code
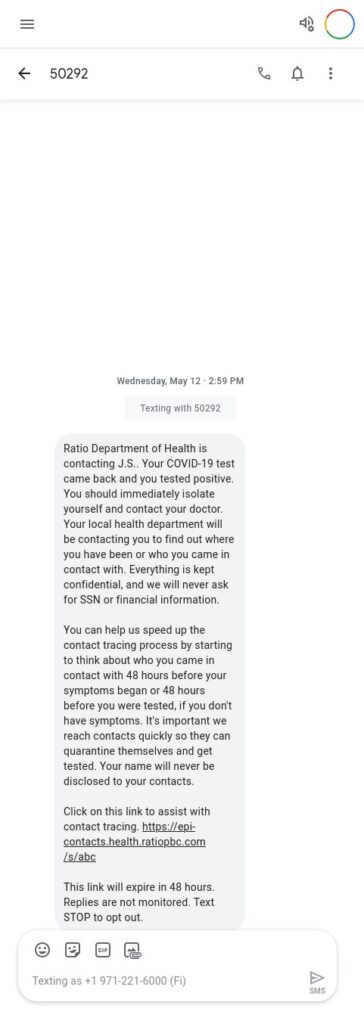
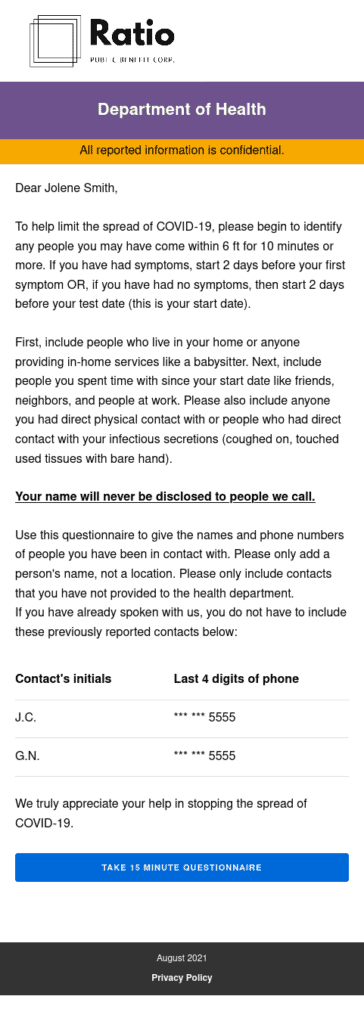
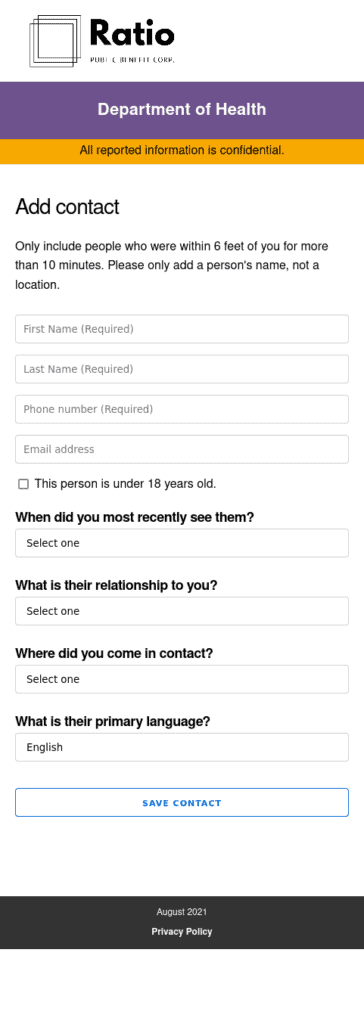
- Epi Contacts is a contact elicitation form that is sent to index cases via SMS directly from case management systems as soon as the Department of Health receives a positive lab result. This improves efficiency and accuracy of case investigation interviewing by enabling cases to self-enter and disclose contact information in a simple web form vs. over the phone. View code
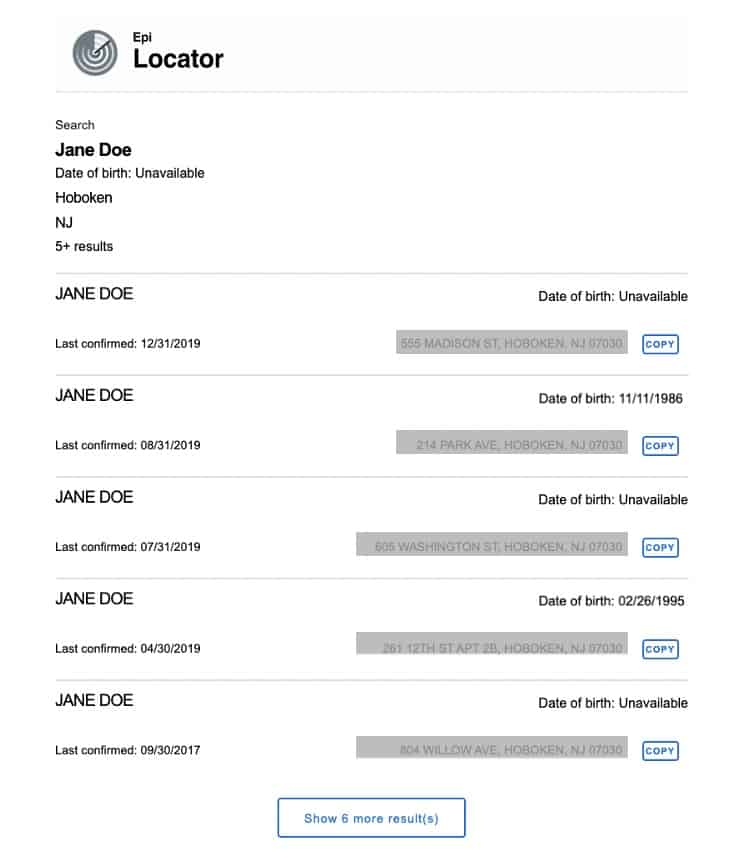
- Epi Locator is a plug-in extension that connects a case management system to third-party investigative look-up tools such as Thomson Reuters. Epi Locator enables contact tracers to more quickly locate critical and missing information —such as a phone number— in order to reach index cases and their contacts. View code
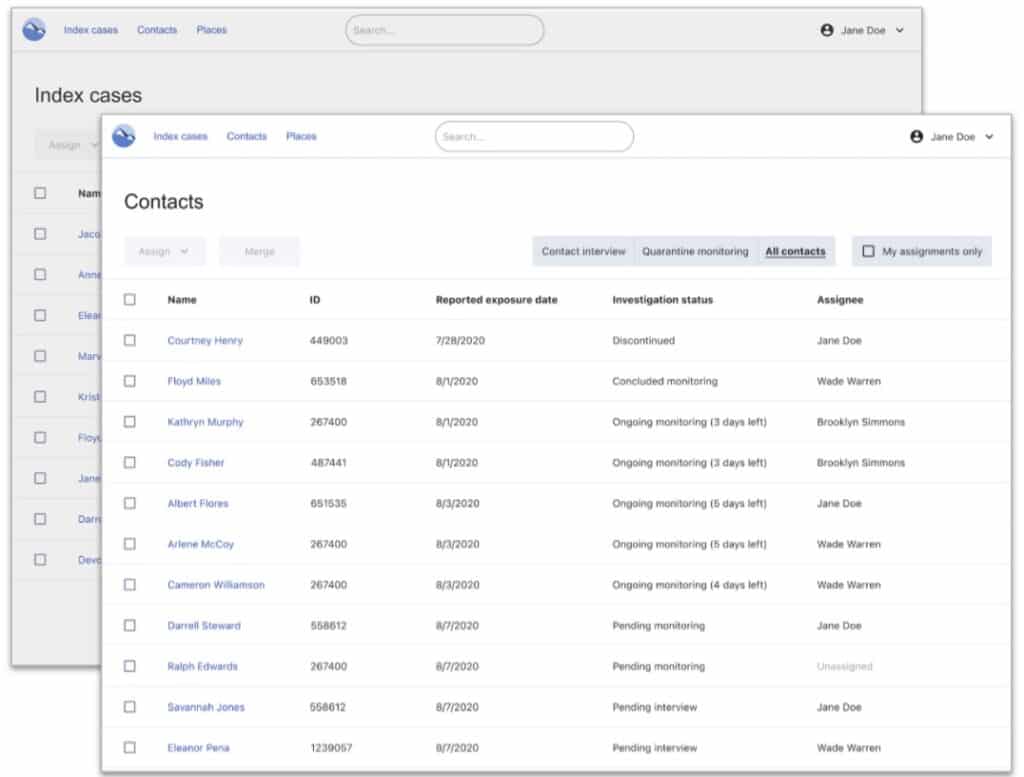
- Epi Viewpoint is a simple and focused case management system designed to enable smaller jurisdictions to quickly and cost-effectively stand-up their contact tracing and case investigation efforts. View code
Lessons Learned: Implementing Software During a Crisis
Focus on optimizing workflows while minimizing change management.
There were thousands of rapidly hired staff members responsible for contact tracing and case investigation in some of the states we worked with. Providing staff with ongoing training in the midst of an overwhelming queue of work-to-be-done presented a significant challenge for our public health agency partners. In some cases, we found that a familiar user experience was more valuable than an improved user experience, because it didn’t require changing the expectations of users.
This lesson presents a key insight into shaping the types of projects that are likely to succeed in a crisis. Two of our most successful projects did not change the core systems or user interfaces that contact tracers and case investigators were using: they simply captured vital data (test result data from labs, contact data from cases) and loaded it into the case management system faster and without manual data entry. These optimizations helped increase the efficiency of the contact tracing workforce without burdening them with additional training.
When shaping projects in the midst of a crisis, it’s important to think through how much change management will be needed, and — where possible — prioritize projects that can deliver value with minimal training requirements.
Align and empower a small, cross-functional team to make decisions quickly.
It’s often the people and organizational complexity (not technology) that make deploying software time-consuming within an enterprise or government organization. Technology decisions have wide-reaching ramifications, so large organizations rightly establish processes that involve many different teams, stakeholders, etc. This approach can be useful to help mitigate risk, but in a crisis, inaction can actually create more risk rather than less.
When speed is critical, it’s important to create a fast-tracked, transparent decision-making process. The process should include enough people with the expertise to make informed, sound decisions — representing disciplines like IT/Security, Program/End User, and Procurement — but should be narrowly focused on who has the authority to say “no” and “yes.” Across the projects we’ve worked on, there were moments in which a lot of stakeholders were present for key discussions, but the team wasn’t able to move forward because the person with the authority to decide was either not present or ambiguously defined. Similarly, we experienced a critical setback to implementation when a stakeholder who had the authority to say “no” was brought in just before scheduled go-live rather than at project inception.
When shaping teams to deliver software in the midst of a crisis, public health leaders can decrease the risks associated with moving too slowly by aligning and empowering a small team that have the expertise to make sound decisions and the authority to act quickly.
Lessons Learned: Preparing Technology Systems Before a Crisis
Build open, well-documented APIs for core public health data systems.
With modern technologies like cloud-based infrastructure and open source web frameworks, we were able to build new digital tools quickly and cost-effectively. However, a business application such as Epi Contacts is not very helpful to public health agencies on its own. New applications need to integrate with one or more core data systems to have a meaningful impact. In our case, we needed to integrate the contact tracing applications with Disease Reporting Systems and Case Management Systems to send and receive COVID-19 test results, case and contact data.
While the modern web has made dramatic advances to integrate separate applications with open, well-documented APIs, many core public health data systems are still largely closed off, making integration a complicated, time-consuming, and expensive proposition. This challenge presents a hurdle to IT modernization efforts during non-crisis times, but it is a critical barrier to effective response during a crisis. Across each of these projects, the biggest barrier to implementing and iterating quickly was integrating with source and recipient data systems.
When evaluating technology systems and vendors for core data systems outside of a crisis, prioritizing open, well-documented APIs as a core requirement can help public health leaders prepare to respond quickly to unknown future needs.
Final Thoughts
Public health agencies play a vital role in supporting the health and well-being of the communities they serve. When a public health crisis occurs, we all benefit from a public health workforce who has the resources and authority to act quickly to minimize the harm that crisis can cause. A small piece of that preparedness includes the capacity to implement and adapt technology quickly based on evolving and emergent needs.
Our experience in the early stages of the COVID-19 pandemic offers lessons for how people (empowered cross-functional teams at jurisdiction partners), processes (minimizing change management), and technology (open, well-documented APIs systems and tools) can work together to support the effectiveness of public health responses. Our hope in sharing these lessons and open-source tools is so that our broader public health and technology communities can continue to build upon these to better prepare for future public health crises.
Resources
Each of the applications discussed here are available on Github under an open source license. For more information about these applications, contact hello@ratiopbc.com.
For more U.S. COVID-19 resources from Resolve to Save Lives, visit https://preventepidemics.org/covid19/us-response/.